Intrauterine artificial insemination (AI or IUI) is a low-complexity assisted reproduction technique. Due to its simplicity, IUI is generally the first option to attempt a pregnancy when a couple has mild fertility problems and goes to an assisted reproduction center.
However, the success rate of AI varies from 5.8% to 13.2% (delivery rate) depending on the woman's age. Therefore, it is very important to meet some requirements to guarantee the maximum chance of success.
Provided below is an index with the 6 points we are going to expand on in this article.
- 1.
- 1.1.
- 1.2.
- 1.3.
- 2.
- 3.
- 3.1.
- 3.2.
- 3.3.
- 3.4.
- 3.5.
- 4.
- 5.
- 6.
Requirements for IUI
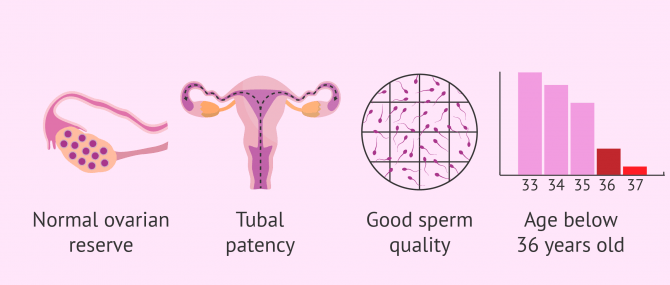
In order to perform an artificial insemination (AI) with the possibility of pregnancy, it is necessary that both the woman and the man (in the case of a male partner) meet a series of requirements. Among these prerequisites for AI are the following:
- Tubal patency
- Good ovarian reserve
- Age of the woman below 36 years old
- Good sperm quality
To check if the woman or couple meet the necessary conditions to carry out artificial insemination, the specialist doctor will indicate the appropriate fertility tests that must be done previously.
In the event that these conditions are not met, it is best to go directly to the in vitro fertilization technique (IVF), since its success rate is much higher than that of AI.
Did you know that we can help you to choose a fertility clinic for your IUI cycle? All you have to do is get your Fertility Report now. It is an easy-to-use tool that is capable of filtering the best clinics and tailor an individual report exclusively for you with useful tips that will help you make a well informed decision.
To follow, we will explain in more detail each of the main requirements mentioned for artificial insemination.
Tubal patency assessment
In IUI, the union of the egg with the sperm, ie fertilization, occurs in the woman's Fallopian tubes. Hence it is essential that the patient's tubes are permeable and functional (or, at least, one of them), to perform an AI that offers chances of success.
The egg is picked up by one of the fallopian tubes after ovulation, where it waits for a sperm to fertilize it. In an AI, the semen sample is deposited directly into the woman's uterus. However, the sperm must subsequently travel on their own to reach the egg in the fallopian tube. Therefore, if the fallopian tubes are blocked, the egg and sperm cannot meet and pregnancy will not occur.
For all these reasons, it is essential to check the patient's tubal patency as a requirement to perform an AI. This procedure can be performed with any of the following techniques:
- Hysterosalpingography
- This is a radiological study of the female reproductive system thanks to the injection of a contrast liquid through the vagina.
- Hysterosalpingosonography
- consists of the introduction of a saline fluid or a foamy gel through the cervix that allows observation of the uterus and tubes by ultrasound.
These tests, in addition, also provide information on possible uterine malformations that could hinder embryo implantation or the development of pregnancy.
You can find more information about these techniques in the following link: What is hysterosalpingography? - Indications and results.
Age and ovarian reserve
As explained above, the maximum age recommended for a woman to undergo IUI is 36 years. From this age on, the success rate starts diminishing dramatically due to a diminished ovarian reserve.
Moreover, regardless of age, all women have to undergo a series of blood tests to get their hormone levels checked, including an AMH test (anti-Müllerian hormone test).
This hormone study, together with a transvaginal ultrasound to perform an antral follicle count, will allow the gynecologist to assess the ovarian reserve and the function of the patient's menstrual cycle.
Sperm quality
Once the semen is deposited in the patient's uterus in an AI, the sperm must be able to reach the egg without any help. For this reason, it is essential that the man has good mobility and sperm concentration so that the intrauterine insemination has a chance of success.
The main test in men that will determine if artificial insemination is possible is the MSC seminogram (Motile Sperm Count). After processing the seminal sample, the MSC obtained must be equal to or greater than 3 million spermatozoa in order to carry out the IUI, that is, there must be at least 3 million spermatozoa that are moving well.
On the other hand, if the only requirement that is not met to perform AI refers to the quality of the sperm, the couple may choose to perform artificial insemination with donor sperm (AI with donor sperm) or go directly to IVF.
Cost of AI
Artificial insemination is one of the cheapest assisted reproduction treatments. Therefore, it is the most chosen option for a first attempt as long as the basic requirements of age, seminal quality, and tubal functionality are met.
The cost of AI varies depending on the assisted reproduction clinic chosen, and in the country where you chose to have the treatment. IN Spain, it usually ranges between 700-1,100€. If you have to resort to a sperm donor, as would be the case of single mothers by choice or female partners, the price of IUI can be up to €1,700. This is due to the necessary financial compensation for the donor.
Costs of artificial insemination in other countries
Artificial insemination prices vary depending on the country where the treatments are performed.
In the United States, artificial insemination costs between $300 - $1,000 without insurance. However, if artificial insemination is performed with donor sperm, the price increases by 900 dollars.
In the UK these figures are approximately £700 - £1600 when paying privately, and an additional £600 if donor sperm is required. However, in some cases treatment may be available on the NHS.
FAQs from users
In female couples, must both sign the informed consent for DAI?
The IAD only requires the medical participation of one of the women of the couple, so the other is not involved in the treatment itself. However, for legal purposes, if both want to be the future parents of the baby, both must always sign the informed consent.
Of course, if that is not their wish, only the signature of the woman performing the treatment will be required.
Is there any difference between the requirements to undergo artificial insemination by husband (AIH) and artificial insemination by donor (AID)?
Intrauterine insemination (IUI) or artificial insemination (AIH) involves the placement of washed sperm into a woman’s uterine cavity using a small catheter during a minor office procedure while the woman is awake.
The sperm are processed in the laboratory to obtain the highest numbers of moving sperm in a small volume as well as enhancing their fertilization potential. The IUI catheter deposits the sperm at a location closer to the fallopian tubes in comparison to intercourse. Following the procedure, the woman can resume all normal activity including intercourse with her partner.
Prior to IUI with partner sperm (AIH) and IUI by donor sperm (AID), the evaluation consists of ensuring the woman ovulates, confirming the fallopian tube(s) is/are open, and the sperm analysis is adequate for IUI. All women desiring pregnancy should undergo prenatal bloodwork including proper blood count, thyroid function, vitamin D level, immunity to the German measles (rubella virus) and chicken pox (varicela virus) as well as an updated Pap smear.
Additional recommendations for women desiring pregnancy with donor sperm include the same infectious disease testing as the donor including cytomegalovirus (CMV) antibody testing. If the woman tests negative for CMV then she needs to select a sperm donor who is also CMV negative to avoid the low but potential risk of infection to the baby. We also advise a psychological counseling session as a consent and for education.
Can I get artifical insemination on the NHS?
The eligibility for IUI on the NHS depends on the area where you live so do check with your local GP.
Notwithstanding, the criteria for treatment on the NHS are:
- An inability to have normal, vaginal sex
- A pre exisiting condition which contradicts unprotected sex, for example one partner with HIV
- same sex couples who have previously many 6 cycles of IUI at a private licensed clinic
Is there any special requirement for a single woman to undergo IUI?
No, a single woman who wishes to become a single mother through AID must meet the requirements already listed above: to have a normal ovarian reserve and tubal patency.
Since donor sperm is used, sperm quality will be excellent and comply with the minimum requirements to being used for an IUI.
Read more: IUI with Donor Sperm – Definition, Process & Success Rates.
Who can use artificial insemination?
Patients who turn to artificial insemination to achieve a pregnancy are those with mild infertility issues, including:
- Mild male factor
- Cervical factor
- Polycystic ovary syndrome (PCOS)
- Unexplained infertility
Moreover, it is the option of choice for single women and lesbian couples, as long as they meet the requirements explained throughout this article.
Recommended readings
As already explained, a woman must have a good egg count for AI to be successful. To learn more about the importance of egg quality and quantity, see also: How Many Eggs Does a Woman Have? – Your Egg Count by Age.
As regards sperm quality, it can be assessed with a basic semen analysis. You can get the details of this infertility test in the following post: What Is a Semen Analysis Report? – Purpose, Preparation & Cost.
We make a great effort to provide you with the highest quality information.
🙏 Please share this article if you liked it. 💜💜 You help us continue!
References
Allen NC, Herbert CM 3rd, Maxson WS, et al: Intrauterine insemination: A critical review. Fertil Steril 44:569–580, 1985.
Alvarez JG: Nurture vs nature: How can we optimize sperm quality? J Androl 24:640–648, 2003.
Keck C, Gerber-Schafer C, Wilhelm C, et al: Intrauterine insemination for treatment of male infertility. Int J Androl 20(Suppl 3):55–64, 1997.
Nuojua-Huttunen S, Tomas C, Bloigu R, et al: Intrauterine insemination treatment in subfertility: An analysis of factors affecting outcome. Hum Reprod 14:698–703, 1999.
Osuna C, Matorras R, Pijoan JI, Rodriguez-Escudero FJ: One versus two inseminations per cycle in intrauterine insemination with sperm from patients’ husbands: A systematic review of the literature. Fertil Steril 82:17–24, 2004.
Plosker SM, Jacobson W, Amato P: Predicting and optimizing success in an intra-uterine insemination programme. Hum Reprod 9:2014–2021, 1994.
Sakkas D, Tomlinson M: Assessment of sperm competence. Semin Reprod Med 18:133–139, 2000.
FAQs from users: 'In female couples, must both sign the informed consent for DAI?', 'Is there any difference between the requirements to undergo artificial insemination by husband (AIH) and artificial insemination by donor (AID)?', 'Can I get artifical insemination on the NHS?', 'Is there any special requirement for a single woman to undergo IUI?' and 'Who can use artificial insemination?'.
Authors and contributors

More information about Michelle Lorraine Embleton
More information about Cristina Algarra Goosman

More information about Michelle Lorraine Embleton







Hi, I have had two AI’s this year and there is no way to get the baby my question is, how many cycles can I do AI before I have to move on to other treatments? Financially we are not able to spend a lot, thanks
Hi Felisha,
When performing AI it is recommended to make a maximum of 4 attempts or cycles, this is because according to recent studies after the 4th attempt the probability of pregnancy does not increase, resorting to another technique such as IVF more appropriate.
I recommend that you talk to your doctor to explain the procedure in the short and long term with all the options you have, whether AI works or not. You could also read the following article on the success rates of AI: How successful is AI?
I hope I have helped you,
Best regards.
Hi, I had an ectopic pregnancy a few years ago and unfortunately had to have a tube removed. Years later I find myself strong enough to give it a try. Is it possible to get pregnant? If not do a fertility treatment like this?
Hello Rachelle,
For a natural pregnancy to occur, among other things, you must have permeable and functional fallopian tubes. If after a year of unprotected sex you have not achieved pregnancy (6 months if you are older than 35 years), I recommend that you go to an assisted reproduction clinic to assess the state of your reproductive system and indicate the most appropriate technique for your situation.
I hope I have helped you,
Best regards.